Achalasia and Esophageal Motility Disorders
Achalasia and Esophageal Motility Disorders
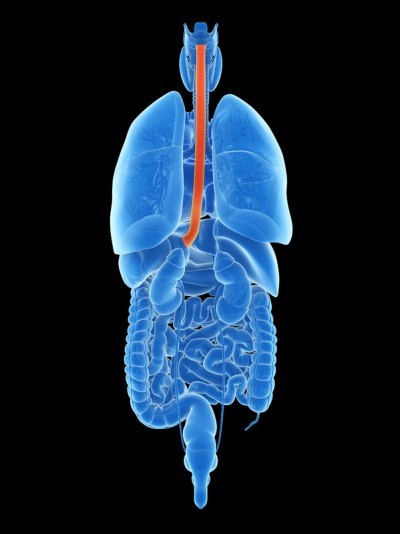
The esophagus (ĕ-sof´ah-gus) is the hollow, muscular tube that moves food and liquid from your mouth to your stomach. If the muscles in your esophagus don’t squeeze properly, it will be harder for the food and liquids to reach your stomach. This condition is known as an esophageal motility disorder. Esophageal motility disorders make it difficult for you to swallow, cause food to come back up into your mouth, and sometime cause chest pain.
One type of esophageal motility disorder is achalasia (ak-uh-lā´-zhuh). Achalasia occurs when the nerves in the esophagus degenerate. As a result, the muscles in the esophagus stop working (no peristalsis), and the valve at the bottom of the esophagus doesn’t open. The condition is believed to affect 1-2 people in every 100,000, with about 3,000 new cases diagnosed each year in the United States.
Other less common dysmotility disorders include spastic esophageal motility disorder (nutcracker esophagus and diffuse esophageal spasm), inefficient esophageal motility disorder, and secondary esophageal motility disorders, which are related to other medical conditions like scleroderma, diabetes, and alcohol consumption.
Causes Of Achalasia
While achalasia can be caused by a parasite in South America (Chagas Disease), in most patients in the United States there is no known cause for their achalasia. Some researchers think it may be linked to a virus.
Recent studies have indicated that achalasia may be caused by an immune disorder in which the patient’s own immune system attacks the nervous system within the muscles of the esophagus, causing them to malfunction.
Achalasia doesn’t affect any particular race or ethnic group, and the condition does not run in families. Esophageal motility disorders develop slowly and worsen over time. If you experience only a brief episode of symptoms, you probably don’t have a true esophageal motility disorder.
Symptoms Of Achalasia
- Dysphagia
- Reflux
- Pressure In The Chest After Eating
Patients with achalasia are sometimes initially treated for gastroesophageal reflux disease (GERD) before being diagnosed with achalasia on further testing.
Symptoms of achalasia include:
- Difficulty swallowing
- Pressure in the chest after eating
- Backing up of undigested food and fluid (regurgitation) sometimes hours after eating
- Coughing or choking on food
- Bad breath
The symptoms can worsen with certain foods (such as meat, bread, and rice), certain liquids (such as carbonated beverages), and eating too close to bedtime.
Left untreated, achalasia can cause considerable weight loss, lung infections, and pneumonia.
Diagnosis And Treatment Options
Tests useful in diagnosing achalasia include high-resolution esophageal manometry, esophagram (barium swallow), and endoscopy.

Barium esophagogram demonstrating marked dysmotility
There is no cure for achalasia, but once you have been diagnosed with the condition, various medications and surgical procedures, performed by a cardiothoracic surgeon, may help treat the symptoms.
The various treatment options are outlined below.
Esophageal Dilation
A balloon or rubber dilator is used with esophagoscopy to stretch the muscles of the lower esophageal sphincter. There is a small risk of tearing or rupturing the esophagus which could require emergency surgery. Sometimes multiple treatments are required based on symptoms. Generally, dilation is recommended for older patients or patients not fit for surgery.
Botox
Botulinum toxin can be injected with esophagoscopy to relax the lower esophageal sphincter for 1-2 months. This becomes less effective over time and repeat injections can cause scarring making surgery or myotomy more difficult in the future. Botox injection is usually a temporary treatment, but response to Botox is reassuring that other procedures to open the lower esophageal sphincter will be successful.
Heller Myotomy
A myotomy is most frequently performed using minimally invasive techniques (laparoscopic or robotic ) using five small incisions although it can also be performed through an open incision in the abdomen or the left side of the chest between the ribs. The surgeon will cut the affected muscles in the esophagus and stomach to make it easier for food to reach the stomach. To reduce the risk of gastroesophageal reflux, a partial valve, or wrap, is created using the stomach (Dor, Toupet, or Transoral Incisionless fundoplication).
Per-oral Esophageal Myotomy (POEM)
Using esophagoscopy, a hole is made from the inside of the esophagus creating a tunnel to divide the esophageal and stomach muscles. The hole is sealed with a clip or suture at the end of the procedure. The long-term results continue to be evaluated. Like dilation, an antireflux procedure (wrap or fundoplication) is not performed with more risk of gastroesophageal reflux once the muscles are divided. POEM is performed by highly specialized gastroenterologists.

Esophagectomy
If you have end-stage achalasia with a severely dilated or tortuous esophagus, opening the lower esophageal sphincter is unlikely to be successful and removal of the esophagus, or esophagectomy, may be recommended. Esophagectomy is usually reserved as a last-resort treatment option.



It is important to remember that no treatment will cure achalasia, but all forms of treatment will help manage symptoms.
Recovery
As with any surgery or procedure, there are risks involved.
If you underwent minimally invasive (laparoscopic) surgery, you should expect to remain in the hospital for 24-48 hours following the procedure. You likely will be able to return to regular activities in about 2 weeks. With open surgery, your hospital stay will be slightly longer but you should still be able to return to normal activities in 2 to 4 weeks.
A barium swallow may be obtained before discharge to confirm that there is no leak and that barium passes through the esophagus easier.
Patients will generally go home on a liquid diet for a few days to weeks slowly progressing to a soft diet and eventually regular diet over approximately six weeks.
It is important to remember that no treatment will cure achalasia, and while swallowing may be much improved, certain foods may still cause dysphagia or regurgitation, and patient should still sleep at an angle to prevent getting food or fluid into their lungs while sleeping.
Talk with your doctor about the best treatment options for you.